Tuberculosis Test Blood Testing, Port Moresby
Question 1. What is tuberculosis?
Tuberculosis (TB) is an infectious disease that develops slowly and can lead to ill health for a long time. If it is not treated it can cause death.
Question 2. How does it occur?
TB is caused by a type of bacteria called Mycobacterium tuberculosis. The bacteria usually attack the lungs. They can destroy parts of the lungs, making it hard to breathe. The bacteria can spread to and damage other parts of the body, especially the brain, kidneys, bones, and joints. The lymph nodes can also become infected.
Most people who are infected with TB bacteria do not develop active TB; that is, they do not become sick and usually do not infect others. Their body defences control the infection by building a wall around the bacteria. However, the walling-in process does not kill the bacteria. If you are infected and later become weak, ill, or undernourished, you may start having active TB. If you are exposed to a large amount of TB bacteria, you may become ill soon after you are infected.
TB is very contagious. It is spread mainly through the air. A person who has active TB can spray droplets infected with the bacteria into the air by coughing, sneezing, or laughing. Tiny particles containing bacteria may stay in the air for several hours, ready to be breathed in by another person.
Question 3. What are the symptoms?
Anyone who has had prolonged close contact with TB infected person should be highly suspicious of TB with the symptoms below. Symptoms of TB can begin anytime from 2 months to several years after you are exposed. Possible symptoms are:
Tiredness
Cough
Neck gland swelling
Under-arm swelling
Weight loss and loss of appetite
Fever
Sweating at night
Joint pain/Lower back pain
A cough that starts out dry but later produces sputum
Blood in Urine
In children other problems include:
Poor growth/weight gain
Recurrent chest infection
Sometimes there are no symptoms.
Question 4. How is it diagnosed?
Your health care provider will ask about your symptoms and give you a physical exam. You will need to have a tuberculin skin test, chest x-ray, and sputum culture: In some cases, biopsy of lymph glands and lung tissue will be done.
Tuberculin (PPD) skin test: Your health care provider will inject a substance called tuberculin, or PPD, beneath your skin. If you are infected with TB, a lump will form where this shot was given within 3 days. This reaction is called a positive tuberculin test. It means that TB bacteria have invaded your body. It does not necessarily mean you have active, infectious TB. In fact, most people with positive tuberculin tests do not have active TB. If your PPD test is positive, close family members should also have the test. However, if you have had TB vaccine in the past, your mantoux can be positive without you having active TB infection. Your doctor will assist you for interpretation. Read more on TB skin or Mantoux Test.
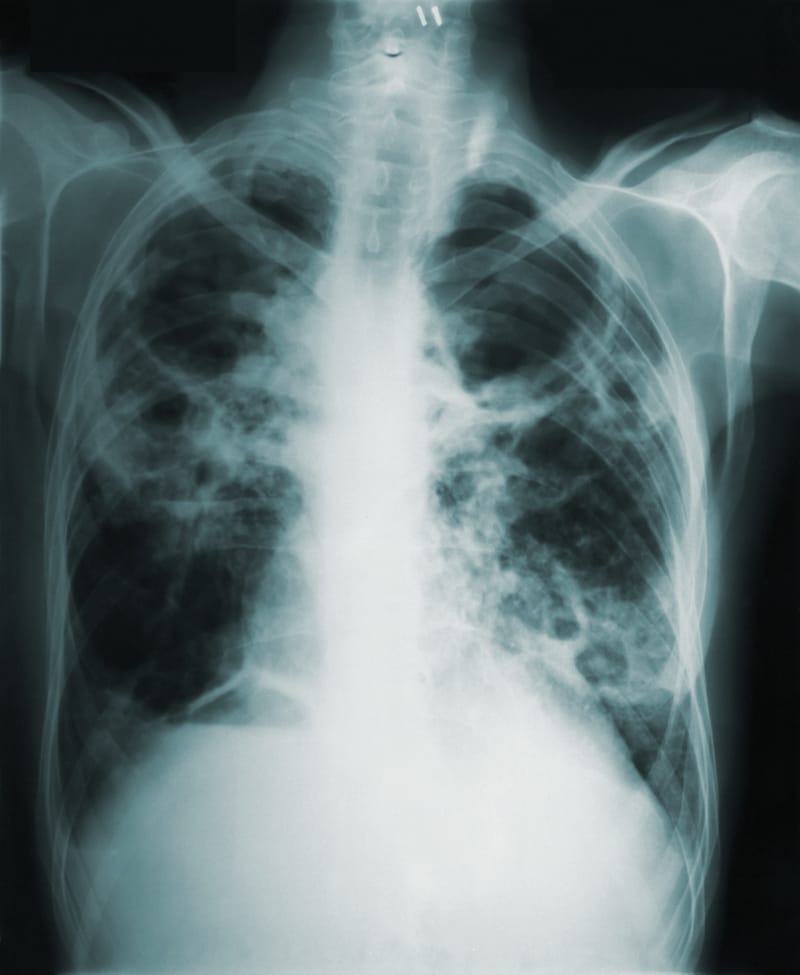
Chest x-ray: If you have inhaled TB bacteria but have fought off the infection, your lungs may not be damaged and your chest x-ray may be normal. However, if you have an active infection and bacteria have attacked your lungs, the damage may be seen on a chest x-ray.
Sputum Check: Sputum is material coughed up from the lungs. It may include mucus and blood. A sample of sputum coughed up from the lungs can be stained with special stain (ZN stain) and viewed under a microscope to see if it contains TB bacteria. A sample of sputum is also used to grow (culture) TB bacteria in the laboratory using special media or bacteria food. A TB bacterium is very slow growing organism & it may take up to 6 to 8 weeks for a sputum culture to give definite results.
Blood Tests: Various blood test are available. Some measure antibody level in blood and others measure specific cells called lymphocyte that has changed its form due to invasion of TB bacteria.
Tissue biopsy: e.g. Lymph glands, pleura (lung tissue), joint tissue
The common tests are sputum, blood and tuberculin (Mantoux) test. Newer tests measuring TB activated lymphocytes in blood are more specific but currently still expensive and requires specialised equipment. Biopsy of infected tissues like lymph glands and lung tissue can be taken to demonstrate signs of TB in the laboratory. (see FNAB)
TB activated Lymphocyte Test.
This test measures subset of lymphocytes specific for Tuberculosis infection. At the time of writing, only 2 tests methods available on the market. One of these tests (Qantiferon) is already being tested in PNG.
Question 5. I had a chest x-ray but my doctor says there is no sign of TB. Can I still have TB?
Yes. In the early stages of lung TB, your chest x-ray may be perfectly normal despite you having pulmonary (chest) TB. Your chest x-ray may also be normal if your TB is extra-pulmonary or outside lung tissue. On the contrary, your chest x-ray may show signs of TB even without you having a cough. Your doctor will often use combination of history (your complaints), examination findings and laboratory tests to decide on your treatment.
Question 6. My sputum check is negative. Can I still have TB?
Yes. You can have TB and yet show negative result on sputum check. To increase your chances of detecting the TB bacteria, multiple sputum checks are often requested. If your doctor suspects that your assessment findings show enough evidence to suggest that you may have TB infection, you will be treated even without positive TB sputum.
Question 7. How is it treated?
If you have active TB, you will be treated with medicines at home or in the hospital. You will probably be given several medicines, which you will need to take for several months. Possible medicines include:
isoniazid (INH)
rifampin
pyrazinamide
ethambutol.
Several medicines are necessary because one alone may not kill all the TB bacteria. These medicines have many side effects and can upset the stomach or cause liver problems. You will need to have regularly scheduled blood tests while you are taking these drugs. Tuberculosis has become an increasingly common disease. New strains of the TB bacteria sometimes cannot be killed by the drugs listed above and new treatments must be found.
Question 8. My doctor has started me on TB treatment without my results. Why is that?
More often when TB is suspected you will be started on treatment immediately even before your results are available. This is very important for lung TB since you are more likely to pass your bacteria to other people around you if left untreated. Tb drugs are then stopped when results show other diseases or if you do not response to treatment.
Question 9. Can I get rid of TB in my system?
Almost all people who are properly treated for tuberculosis are cured. The main reason that treatments sometimes do not work is that people do not take their medicines properly.
Question 10. How can I take care of myself?
Ask your health care provider the following questions:
May I continue doing everything I am used to doing; for example, exercising and cooking for my family? May I continue to work?
What kind of diet is best?
How long after I begin taking the medicines am I still contagious?
If I am pregnant or breast-feeding, will the TB bacteria infect my child? Will the medicines hurt my child?
How can I help protect my family and friends from getting infected?
What are the side effects of the medicines?
Are there any medicines I should avoid while taking the TB medicines?
Can I drink alcohol while I am taking the TB medicines?
What tests should I have before I begin the TB medicines (for example, liver function test)? How often will I need to repeat the tests while I am taking the medicines?
Question 11. What can be done to help prevent tuberculosis?
TB can be prevented. To help prevent the spread of the disease people infected with TB bacteria must be diagnosed early.
If you have active TB, you can help prevent spreading the disease by following these guidelines:
Start treatment with antibiotics as early as possible and take all of your anti-tuberculosis medicine as prescribed.
Dispose of used tissues in a plastic bag and seal the bag before you throw it in the garbage.
Cover your mouth and nose when you cough, sneeze, or laugh.
Wash your hands after sneezing or coughing or anytime your hands are around your mouth or nose.
If you are infected but do not have active TB, you may take isoniazid to prevent an active infection. If you cannot take preventive medicine, make sure you keep your follow-up appointments with your health care provider. Check-up will detect TB that is becoming active. The active TB can then be treated at an early stage before much damage is done.
If you work in a prison, hospital, or long-term care facility, you should be tested for TB regularly. Check with your provider to find out how often you should be tested. You should also ask how often you should be checked if you have a medical condition that weakens your immune system, such as diabetes or HIV infection.
Question 12. I have completed TB treatment but I am still coughing up thick sputum. Do I still have TB?
It is very likely that your TB is cured if you have completed your medication. Occasionally, TB bacteria may develop resistance to the drugs or you may get re-infected. In this case, you may need your sputum checked again in the laboratory to see if you carry any resistant TB bacteria. More often productive cough after pulmonary TB may be due to damage done to your lungs by TB causing bronchiectasis or chronic lung disease. Only occasionally you may have infection with fungus (aspergillus) following lung damage by TB. See your doctor for review and advice on treatment.
Your doctor may request for a repeat sputum check to ensure that you are cleared of TB.
Question 13. I completed TB treatment. Can I have another PPD Skin test (mantoux) to make sure I am cleared of TB infection?
No. Mantoux test will be positive in someone who has had TB before. Mantoux test is only useful to assist diagnosis if you have TB for the first time. Mantoux reaction will remain positive once you have had TB even after treatment or following TB vaccination.
You can only repeat sputum test to ensure that you do not have TB again.


